Electrosurgical units (ESUs), commonly known as electrosurgical equipment, are widely used in surgical procedures. By generating heat through high-frequency electric current, they enable precise tissue cutting and effective hemostasis. Due to their ease of use, rapid cutting, and reliable bleeding control, ESUs have become indispensable tools in operating rooms, particularly in general surgery, gynecology, and colorectal surgery [1]. With the advancement of medical technology, the performance of electrosurgical units continues to improve, significantly enhancing both safety and efficiency, and supporting minimally invasive surgery and faster postoperative recovery.
Compared with traditional scalpels, electrosurgical units can effectively reduce intraoperative blood loss, shorten surgery duration, and lower the risk of postoperative complications. Studies have shown that proper use of ESUs can significantly improve surgical outcomes. In one study involving 160 surgical patients, the observation group receiving care with standardized electrosurgical unit procedures had an average surgery time of 132.9 minutes, intraoperative blood loss of 43.7 mL, and nursing satisfaction of 95.1%, all of which were superior to the conventional care group (P<0.05) [2]. This indicates that scientific usage and comprehensive nursing support are key to maximizing the advantages of electrosurgical units.
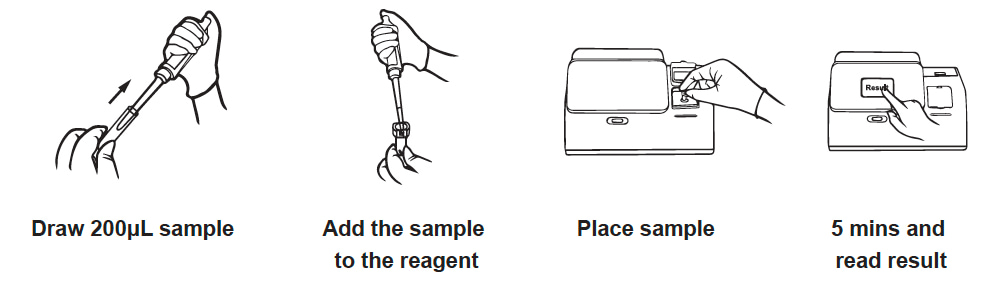
Safe use of electrosurgical units relies heavily on standardized nursing coordination. Nursing staff should check equipment status, electrode placement, and power connections before surgery to ensure a safe operating environment; during surgery, they must closely monitor the patient’s vital signs and equipment performance, addressing any anomalies promptly [3]. For example, selecting the appropriate output power, preventing patient contact with metal surfaces, and using insulation protection can effectively prevent burns and other accidents, ensuring smooth surgical procedures.

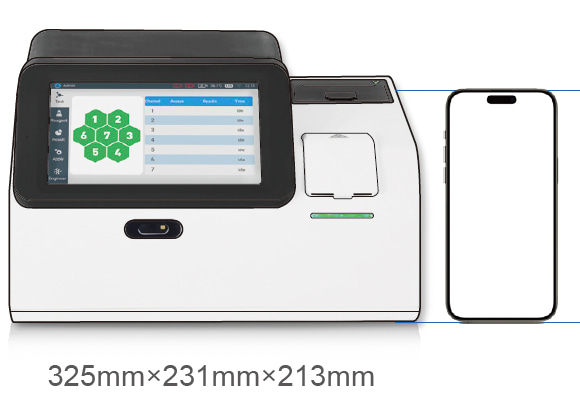
The SEH80A electrosurgical unit from ShouLiang-med integrates multiple intelligent technologies to further enhance surgical safety and efficiency. The device offers 8 monopolar and 6 bipolar modes to meet various surgical needs; its intelligent tissue-sensing function can adjust output power in real time, reducing smoke and eschar formation; and the return electrode monitoring system ensures patient safety from multiple dimensions. Additionally, the SEH80A supports laparoscopic interfaces, is compatible with smoke evacuators, and integrates into modern operating rooms, making it suitable for a variety of complex surgical scenarios and reflecting the efficiency and flexibility of modern surgical equipment.
In summary, electrosurgical units play a crucial role in modern surgery due to their significant intraoperative advantages and integration with proper nursing care. The application of advanced devices like the SEH80A from Shouliang-med has significantly improved surgical precision and safety, effectively promoting minimally invasive surgery and faster patient recovery.
References:
[1] Yan Weidong, Fan Li, Chen Hua, et al. Analysis of Nursing Coordination for the Safe Use of Electrosurgical Units in the Operating Room [J]. Medical Frontiers, 2016, 6(31): 286-287.
[2] Xiao Yingmei. Application Effect of Nursing Coordination for Safe Use of Electrosurgical Units in Surgery [J]. Medical Equipment, 2021, 34(4): 130-132.
[3] Long Yanli, Du Lin. Nursing Coordination for Safe Use of Electrosurgical Units in the Operating Room [J]. Medical Equipment, 2019, 32(10): 146-147.